
Most of us can remember running around barefoot when we were young. Shoes seemed like such a hindrance! As we get older though, shoes are a necessity for overall health and mobility. And while good fitting shoes are important, many foot maladies are often caused by boney prominences consistent with underlying foot deformities. These deformities along with thinning skin layers can increase the risk and frequency of calluses.
What Are Calluses And What Causes Them?
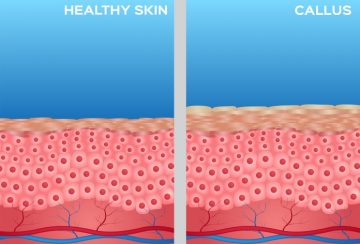 Calluses are thick, hardened layers of skin that develop when the skin tries to protect itself against friction and pressure. Your skin will develop a thick rough patch first and then become a hardened bump which can vary in size. It may become tender or painful to touch and your skin may be flaky or dry.
Calluses are thick, hardened layers of skin that develop when the skin tries to protect itself against friction and pressure. Your skin will develop a thick rough patch first and then become a hardened bump which can vary in size. It may become tender or painful to touch and your skin may be flaky or dry.
Underlying foot deformities such as hammertoes, bunions, or plantarflexed metatarsals can increase the risk of developing calluses. When you have an underlying problem, simply scraping the callus away doesn’t solve the problem. The callus will return because of the constant pressure and friction associated with the deformity. Also, as we age, our skin can become thinner. Diabetes or other health conditions can also cause poor blood flow to your feet and put you at greater risk for calluses.
Calluses most often happen on the feet, but they can also occur on the hands, elbows, or knees. Most health problems don’t have any advantages. Athletes will tell you that calluses do protect and make their feet less sensitive during sports. If you still go barefoot a lot, you have an even greater chance of developing calluses because of the constant bare contact with the ground and the weight you put on your feet (1.5 times your body weight when walking, 7.5 times your body weight when running).
Home Treatment Options
Once you get a callus, there are many at-home treatment options available, including:
- Keeping your feet clean and using a scrub brush to get rid of any excess skin
- Use a moisturizer designed for feet
- Use a pumice stone or a file for your feet to remove harder skin deposits
- Wear socks that fit well
- Use toe separators, felt pads and non-medicated pads or bandages over areas that rub
- Wear properly fitted footwear
It cannot be overstated that wearing ill-fitting shoes when you have underlying foot deformities will cause and exacerbate the formation of calluses and other foot maladies. Shoes that are too tight or too loose, high heels and even seams inside your shoe can cause rubbing and friction leading to foot problems.
In Office Treatment
It’s important that you not try to treat a callus if you have diabetes or other arterial disease. For patients without diabetes, most calluses are unsightly and can lead to a lot of discomfort, but by eliminating the source of friction that causes the callus, the callus can be treated. Often, patients can come in to the office and have their callus debrided (or removed) every six weeks to bring relief. Custom made orthotics with customized depressions or cut outs can redistribute pressure on the feet and can also provide relief, and in-office acid treatments may also be a consideration if patients do not have health issues that make this type of therapy too risky.
This article is part of the Discussion Series on Running Injuries. Please feel free to Contact Us with any questions or you can Make An Appointment to see Dr. Caruso.